Women’s Health in Rural and Underserved Areas: Challenges and Solutions
Women in rural and underserved areas face unique health challenges due to limited access to healthcare services, socioeconomic barriers, and geographic isolation. This blog post explores these challenges, highlighting disparities through statistics, personal stories, and expert insights. We discuss the impact of limited healthcare access on maternal health, chronic conditions, and mental health. Learn about the role of telemedicine and community health workers, and discover policy recommendations aimed at improving health outcomes for women in these communities.
10/5/20243 min read
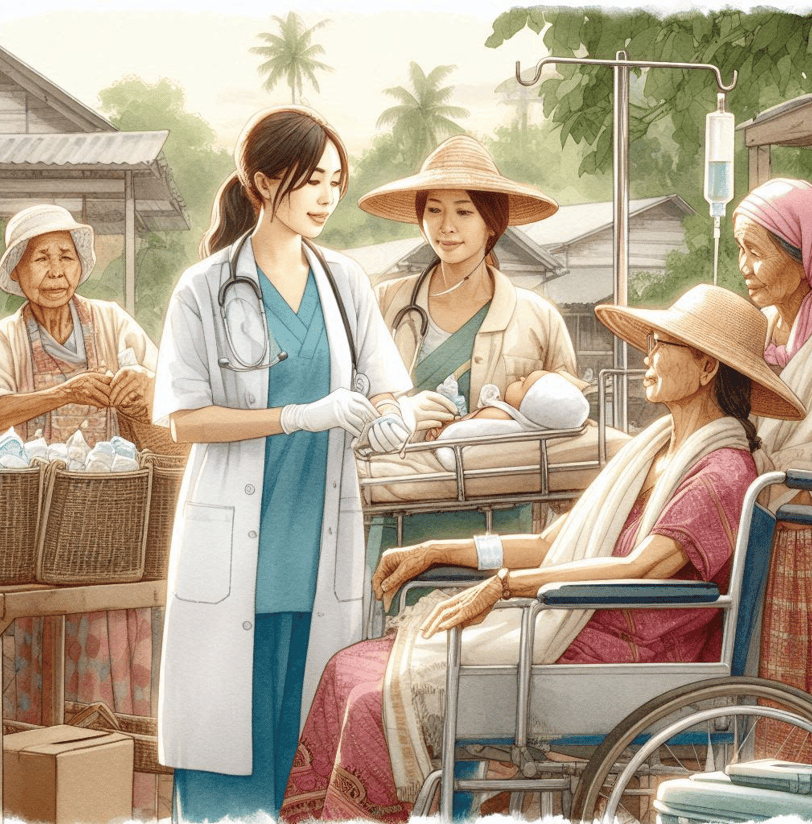
Women living in rural and underserved areas face unique health challenges due to limited access to healthcare services, socioeconomic barriers, and geographic isolation. This post explores these challenges, highlights disparities, and discusses potential solutions to improve health outcomes for women in these communities.
Common Health Issues in Rural and Underserved Areas
Maternal Health: Women in rural areas have higher rates of maternal mortality and complications during pregnancy and childbirth compared to their urban counterparts.
Chronic Conditions: Higher prevalence of chronic conditions such as diabetes, hypertension, and heart disease due to limited access to preventive care and health education.
Mental Health: Increased rates of mental health issues, including depression and anxiety, exacerbated by isolation and lack of mental health services.
The Impact of Limited Access to Healthcare
Healthcare Providers:
Shortage of Specialists: Rural areas often lack specialists, including obstetricians and gynecologists, leading to delayed or inadequate care.
Primary Care Access: Many rural women rely on nurse practitioners and primary care physicians who may not have specialized training in women’s health.
Healthcare Facilities:
Hospital Closures: Rural hospitals are closing at an alarming rate, further limiting access to emergency and specialized care.
Transportation Barriers: Geographic isolation and lack of public transportation make it difficult for women to access healthcare facilities.
Stories and Interviews
Story 1: Sarah, a 32-year-old woman from a rural town, struggled to find prenatal care during her pregnancy. The nearest hospital with maternity services was over an hour away, and she had to rely on a local clinic with limited resources. Her story highlights the critical need for accessible maternal healthcare in rural areas.
Story 2: Maria, a 45-year-old woman living in an underserved urban area, faced challenges managing her diabetes due to the lack of nearby healthcare providers. She found support through a community health worker program that provided education and resources. Her experience underscores the importance of community-based health initiatives.
The Role of Telemedicine and Community Health Workers
Telemedicine:
Access to Specialists: Telemedicine can bridge the gap by providing remote consultations with specialists, reducing the need for travel and increasing access to care.
Mental Health Services: Telehealth platforms can offer counseling and mental health support, which is crucial for women in isolated areas.
Community Health Workers (CHWs):
Health Education: CHWs provide essential health education and support, helping women understand and manage their health conditions.
Advocacy: CHWs advocate for patients, helping them navigate the healthcare system and access necessary services.
Strategies for Improving Women’s Health in Rural and Underserved Areas
Telehealth Services: Expanding telehealth can provide remote consultations and follow-up care, reducing the need for travel and increasing access to specialists.
Mobile Health Clinics: Deploying mobile clinics can bring essential healthcare services directly to rural and underserved communities.
Policy Advocacy: Advocating for policies that increase funding for rural healthcare infrastructure and support the training and retention of healthcare providers in these areas.
Community Engagement: Involving local communities in health planning and decision-making to ensure that services meet their specific needs.
Expert Insights
Dr. Emily Carter, a public health expert, emphasizes, “Improving women’s health in rural and underserved areas requires a multifaceted approach. We need to invest in healthcare infrastructure, support community health workers, and leverage technology to bridge the gap in access to care.”
Statistics on Healthcare Access and Outcomes
Maternal Mortality: Women in rural areas are 60% more likely to die from pregnancy-related complications compared to those in urban areas.
Chronic Conditions: Rural women have higher rates of chronic conditions such as diabetes (17%) and hypertension (25%) compared to urban women.
Mental Health: Approximately 20% of women in rural areas report experiencing frequent mental distress, yet only 10% receive adequate mental health services.
Conclusion
Addressing the health disparities faced by women in rural and underserved areas is crucial for achieving health equity. By implementing innovative solutions and supporting community-based initiatives, we can improve health outcomes and ensure that all women have access to the care they need.
